In our house, if you ride your bike or scooter without your helmet, the bike or scooter goes into time out for 24h. It’s only happened once, but the lesson was learned. Thank goodness, the girl will not ride without her helmet! Did you know that fewer than 25% of bicyclists wear helmets? Nine out of ten people killed in bike accidents were not wearing helmets (Helmets on Heads)? It seems logical that helmets should be worn, but perhaps the best way to learn the importance of wearing a helmet is to watch your child fly down a hill, lose control and land on her head. I can still see the crash in slow motion. She landed on her face. It was terrifying, but I was so thankful when she called for me just after impact. I know the story would be very different if she hadn’t taken that extra 30 seconds to strap on her helmet!
This is the hill that she decided to attempt on the scooter! She crashed right at the bottom (not my photograph).

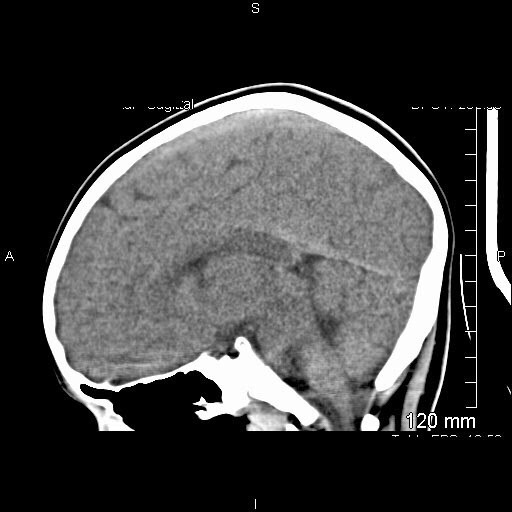
This was the result:

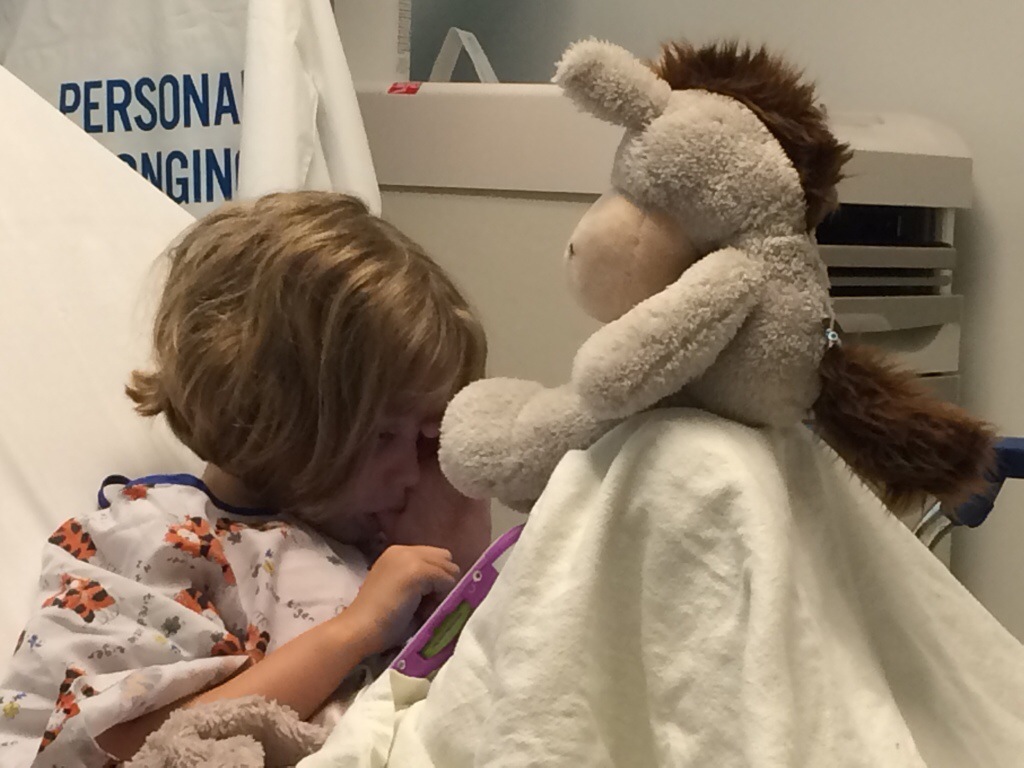
So now she has a concussion and it’s not fun. I have read more student papers on concussions than I ever wanted to read, but I still feel like I don’t understand what’s happening at all! First of all, a concussion is not a bruised brain (like it was described when I was a kid). It’s a traumatic brain injury that changes the functioning of the brain (CDC, Lurie). Most concussions occur without loss of consciousness, and all of them are different. Many are accompanied by a headache, personality changes, problems with memory or concentration, issues with balance and light/noise sensitivities (CDC). The girl had a headache the first two days, but recently her most common complaint is dizziness. I can tell it’s bothering her. She doesn’t want to close her eyes to go to sleep because she feels like she’s falling. She’s also sensitive to light and forgets things.
The treatment for a concussion is “brain rest.” It’s easier to tell you what she can do, rather than list the things that aren’t allowed. The nurse told me that ideally the girl would lie on the couch all day with her eyes closed. Right! She is not allowed to look at any kind of screen (TV, computer, leap pad). She also can’t practice her cello, play the piano, run, jump, spin, ride her bike or scooter, climb trees, or swing. Our original plan (approved by her doctor) was to go to one hour of VBS and one hour of choir camp, but she hasn’t been able to do that much. Keeping her from thinking is the biggest challenge!
I have been reading to her. We are almost finished with book 5 of the Boxcar Children, and we’ve also enjoyed Mercy Watson and her children’s Bible. Yesterday we tried Play doh.

She just can’t play without a lot of thought! Check out this play doh bathroom:

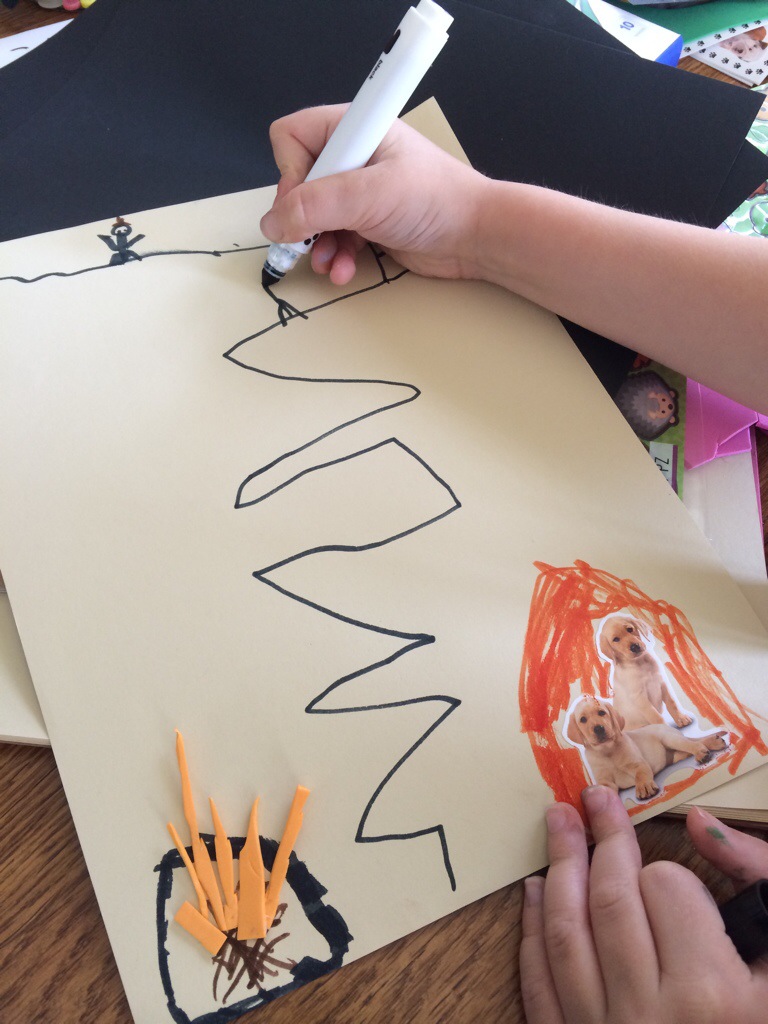
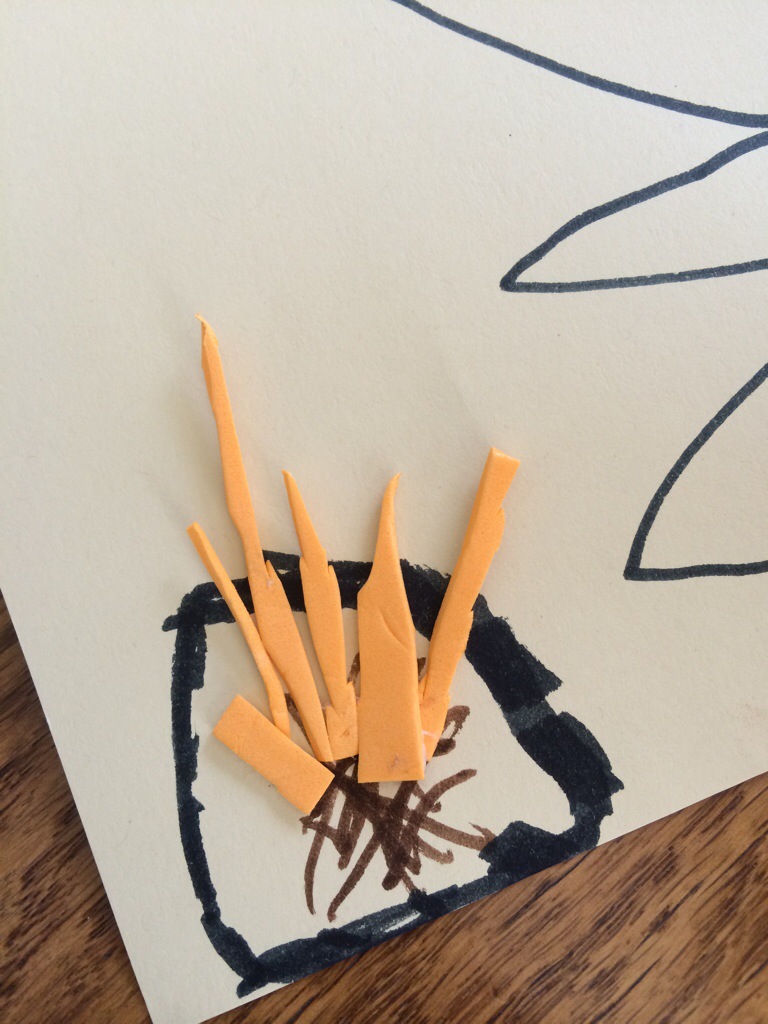
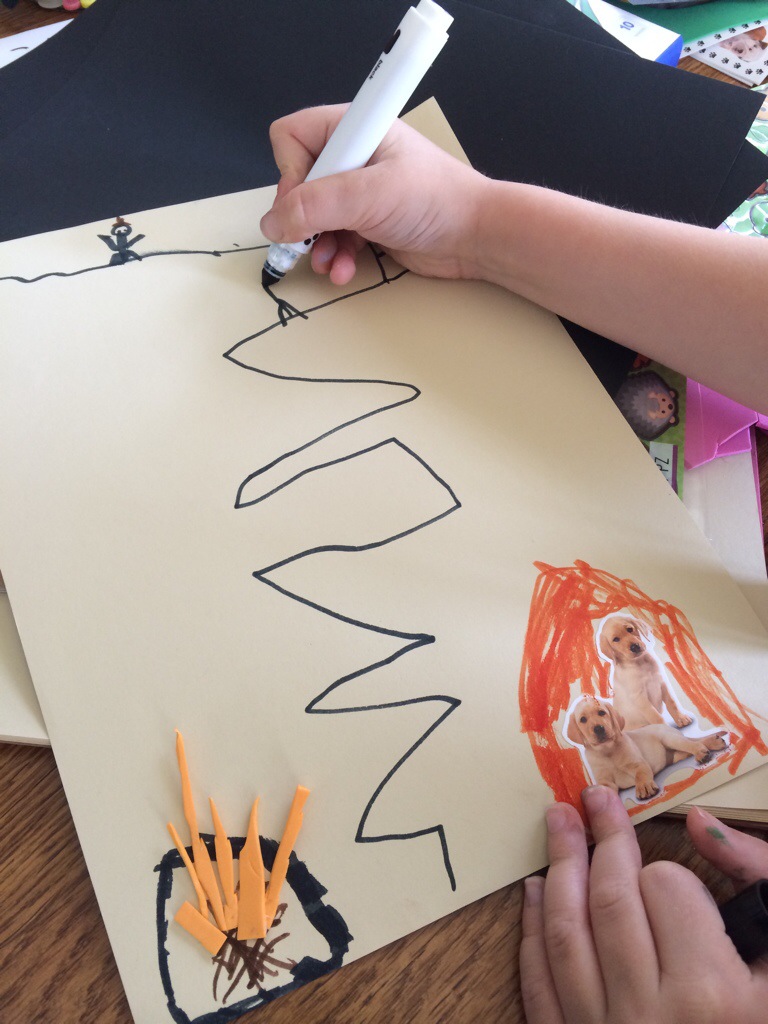
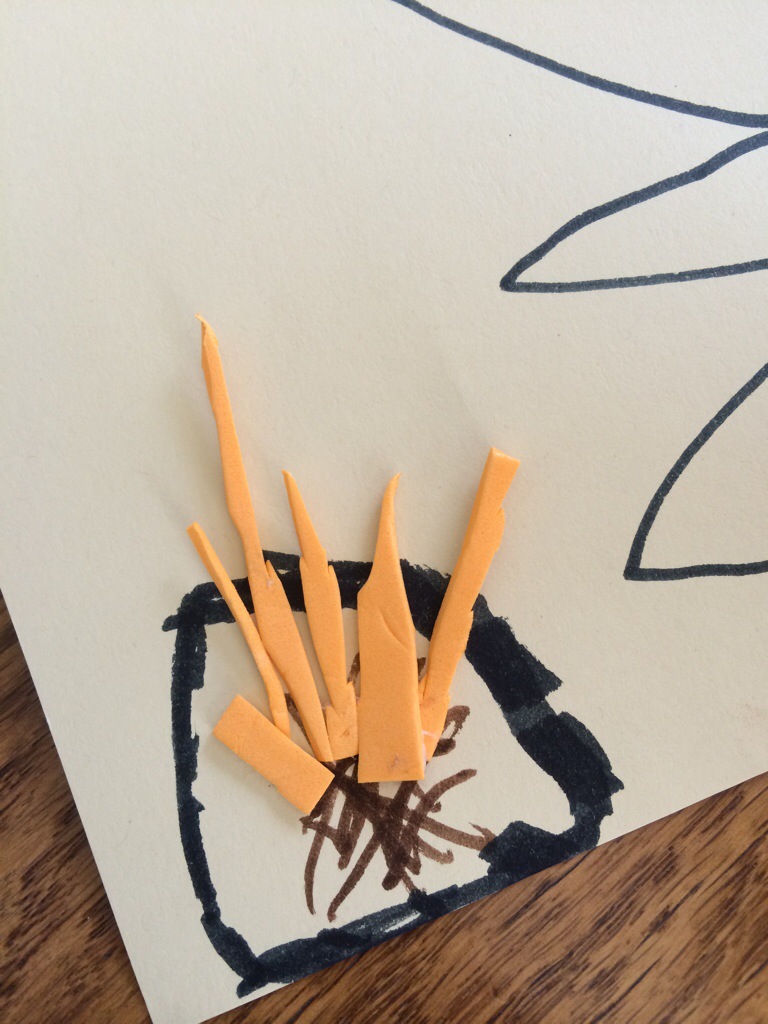
A friend suggested that she cut paper and glue it together without thinking, and she would be surprised by the design. Look at what she came up with! I’m pretty sure she was “thinking” about this design and this fish and the campfire wasn’t simply a surprise.

We have enjoyed blowing bubbles, but it’s really hard to avoid chasing after them! (These photos were taken before the crash, but too fun not to use).


Today we just needed to get out of the house, so we played “Scavenger Hunt.” The girl picked things for me to find while we were out driving. We started with a new train station to the East.

Thankfully, we’ve never actually gotten on or off of the Metra in Lombard. Otherwise, I would have had to drive much further. The next instruction was for me to take her to an airport. We went to the DuPage County Airport rather than driving to Midway or O’Hare.

The last destination was a Target store. Thank goodness she was tired of the game after an hour and a half!

We see her neurosurgeon on Monday. Hopefully she will be doing better by then and we will just have good news! She really wants to be able to play with her new leap pad! That would be the best day ever!
Here’s to helmets! Never Ever Go Without!!!

Sources:
http://www.cdc.gov/concussion/sports/
http://www.helmetsonheads.org/facts/
https://www.luriechildrens.org/en-us/care-services/conditions-treatments/concussion/Pages/index.aspx